It’s estimated that at least 50 million people in the United States suffer from sleep disorders. They range from the mildly inconvenient to the potentially fatal, and at PeaceHealth United General Medical Center in Sedro-Woolley, the hospital’s Sleep Medicine Center provides a host of studies and treatments to put those with sleep disorders on the path to a better night’s rest.
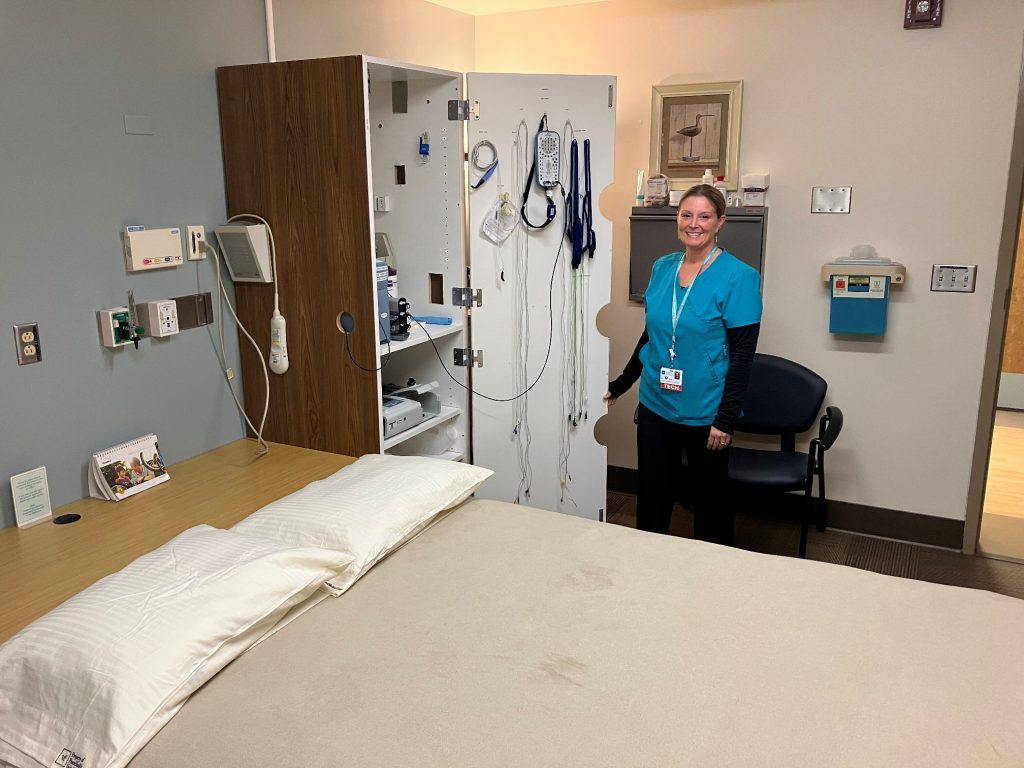
Allison Wilhonen, supervisor of respiratory therapy, says the two-bed facility recently expanded its capacity for in-clinic sleep studies from three to six nights a week and now sees patients per week on average 12, essentially doubling its total volume month-to-month, Wilhonen says.
The center is fully-accredited by the American Academy of Sleep Medicine and has three full-time, board-certified sleep technologists – two at night and one during the day – along with another who works on a per diem basis.
Common Sleep Disorders
Dr. Don Berry, a doctor of sleep medicine for PeaceHealth, says the most common sleep disorders are sleep apnea and insomnia, followed by conditions like restless leg syndrome, hypersomnia (narcolepsy) and various circadian rhythm disorders.
The most common type of sleep apnea is obstructive, where a person’s tongue may be enlarged or relax enough to cover over the airway while sleeping, or their soft palate may be enlarged, causing the airway to frequently obstruct while sleeping. In either case, this can cause snoring and gasping for air.
As a result, patients frequently awaken during the night, even if only briefly. Sue Moore, the sleep center’s daytime sleep technologist, says some people who think they have insomnia may have obstructive sleep apnea, due to waking so often.
People are frequently referred to Berry or one of his colleagues in sleep medicine because their sleeping partners are witnessing loud snoring and/or periods of stopped breathing.
Sleep apnea’s interruption to restful sleep cycles can lead to sore throat, dry mouth, morning headaches and excessive daytime sleepiness, negatively impacting a person’s waking life. Patients with obstructive sleep apnea have an elevated risk of heart attack, stroke, diabetes and other concerns if left untreated.
Central sleep apnea – where the brain fails to send proper signals to the muscles that control breathing – is rarer that obstructive sleep apnea and can be treated with positive airway pressure therapy.
In-Home Sleep Studies in Skagit County
At the United General sleep center, sleep apnea makes up the bulk of sleep studies, which are split into at-home and in-lab observation.
With at-home sleep studies – generally only done for potential sleep apnea cases – a patient comes in for a roughly 10-minute appointment to learn how to use the equipment they’ll take home. This consists of a nasal cannula, a chest belt and pulse oximeter for their finger, Moore says. The goal is to examine the respiratory part of someone’s sleep pattern for a minimum of six hours.
“We don’t collect any information on brain waves,” she says. “It’s solely recording airflow, heart rate, oxygen levels and positions. So, if you’re sleeping on your back versus your side, we can determine the severity of respiratory events on a positional basis.”
Patients bring the equipment back the next available day. Patients in the San Juan Islands can opt for receiving and returning equipment via mail.
After each study, a technician notes each apnea on a graph-based readout of the data. That data is then sent to a doctor for interpretation and formal diagnosis. The diagnosis is sent back to Moore or another provider, who contacts the patient with next steps.

In-Lab Sleep Studies at PeaceHealth United
If a patient has co-morbidities or particularly alarming at-home sleep study results, they are brought into the lab for an overnight study. Here, patients are hooked up to wires and monitored to measure brain waves (EEG) for stages of sleep and heart rhythms (EKG) to check for arrhythmias. They will have belts around their chest and stomach to measure their effort to breath and leg sensors to monitor, leg movements.
Although falling asleep while connected to numerous wires would seem challenging, Moore says that’s surprisingly not the case.
“Patients generally fall asleep within 10 minutes of their sleep study,” she says. “We really do our best at trying to relax the the patient while we’re hooking them up. Sometimes they’re so aware of the wires that they feel like they didn’t sleep well, but we’re monitoring their brain waves; we can tell when they’re sleeping and when they’re not.”
Moore recommends patients bring a change of overnight clothing and any nighttime medications for in-lab studies. They can also take a sleep aid like melatonin if desired, or bring white noise machines – provided they don’t interfere with other equipment.
United General also conducts Multiple Sleep Latency Tests (MSLTs), which can be used to diagnose narcolepsy and idiopathic hypersomnia – two disorders characterized by excessive daytime sleepiness. The MSLT takes 24 hours, Moore says.
Patients must have regular nighttime sleep monitoring to rule out other disorders, before taking 5, 20-minute daytime naps, scheduled 2 hours apart. If sleep is achieved in that window, patients sleep for 15 minutes before being awakened. Depending upon the resulting sleep cycle data, narcolepsy may be diagnosed.
CPAP Treatment for Sleep Disorders
For many sleep apnea patients, treatment consists of using a Continuous Positive Airway Pressure device, or CPAP. The device blows air into a person’s airway in order to keep it from closing.
Those with more severe apnea issues may need a bi-level positive airway pressure (BiPAP) device that blows air both in and out of a patient’s airway, essentially ventilating them, Berry says.

A CPAP is usually covered by insurance as long as patients remain “compliant,” Moore says, using it at least four hours a night and having a follow-up appointment within 90 days. Because CPAP masks are often difficult to get used to, the sleep clinic provides free mask fittings, where Moore is happy to help patients find the most comfortable fit for their machines.
PeaceHealth’s Tips for Better Sleep
Regardless of whether you have a sleep disorder, Berry says there are always things a person can do to ensure a better night’s sleep.
While regular aerobic exercise is healthy and can help you fall asleep easier, anything strenuous should be avoided several hours before bed. Caffeine should be avoided after noon for those with insomnia, as should irregular sleep and wake cycles.
Alcohol is also a no-no in the hours before bed: while it can help someone fall asleep, it often worsens sleep quality later in the night. Once you’re in bed, you should also put down your phone: Berry says studies show that the closer a phone is to a person’s eyes, the more it seems to impact the body’s wake center.
Finally, don’t consume upsetting content right before going to bed, opting for activities like reading. “Try to spend the last hour or so before bed preparing for bed and doing something that’s relaxing for you,” he says.
While nobody – Dr. Berry included – wants you to have sleeping issues, PeaceHealth United General’s Sleep Medicine Center is here to help you figure them out and get back to the rest you deserve. If you think you may have a sleep disorder, speak with your primary care provider about getting a referral.
For more information, call the Sleep Center at 360-856-7533.
Sponsored



































